Air pollution is a significant public health concern, with both short and long-term exposure causing increased morbidity and excess mortality. In 2019, air pollution was the largest environmental risk to health, causing approximately 7 million premature deaths worldwide annually. Of these deaths, about 4.2 million were attributed to ambient (outdoor) air pollution in both cities and rural areas, primarily due to exposure to fine particulate matter, which leads to cardiovascular and respiratory diseases and cancers. WHO data reveals that 99% of the global population breathes air that exceeds the recommended guideline limits, with low- and middle-income countries experiencing the highest exposures and consequent health risks. The health impacts of air pollution are closely tied to socioeconomic conditions, with individuals of lower socioeconomic status (SES) facing increased vulnerability to its harmful effects due to various factors.
| Characteristics | Values |
|---|---|
| Number of deaths caused by air pollution per year | 4.2 million (2019 estimate) to 7 million |
| Percentage of people who breathe air containing high levels of pollutants | 90% |
| Number of people exposed to dangerous levels of household air pollution | 2.4 billion |
| Percentage of global deaths from non-communicable diseases that may be attributed to environmental risk factors | 20% |
| Percentage of the above deaths caused by ambient air pollution | 50% |
| Percentage of global air pollution-related deaths that occur in high-income countries | 20% |
| Percentage of global air pollution-related deaths that occur in low- and middle-income countries | 89% |
| Ambient air pollution-related deaths in China and South Asia | 50% |
| Ambient air pollution-related deaths in WHO South-East Asia and Western Pacific Regions | N/A |
| Ambient air pollution-related deaths caused by ischaemic heart disease and stroke | 68% |
| Ambient air pollution-related deaths caused by chronic obstructive pulmonary disease | 14% |
| Ambient air pollution-related deaths caused by acute lower respiratory infections | 14% |
| Ambient air pollution-related deaths caused by lung cancer | 4% |
What You'll Learn

Cardiovascular and respiratory disease
Ambient air pollution is a mix of solid particles and gases that endangers human health worldwide. Cardiovascular disease (CVD) is a general term for conditions affecting the health of the heart or blood vessels. It is the leading cause of death in the United States, with most deaths occurring in people over 65. In 2016, ambient air pollution was responsible for an estimated 4.2 million deaths worldwide, accounting for about 17% of ischaemic heart disease and 25% of stroke deaths globally. Fine particulate matter (PM2.5), with diameters of less than 2.5 µm, can increase the risk of cardiovascular events. Research has shown that exposure to increased concentrations of PM2.5 over a short period can trigger cardiovascular disease-related heart attacks and death. Longer-term exposure can lead to an increased risk of cardiovascular mortality and decreased life expectancy.
Several hundred epidemiological studies have linked air pollution to human illnesses, with many pollutants causing disease individually or in combination. While the United States has experienced improved air quality and reductions in PM2.5 in recent years, there are still many people exposed to high levels of this pollutant. Evidence suggests that populations with underlying cardiovascular conditions or previous cardiovascular events may be at increased risk of PM2.5-related health effects. Additionally, people exposed to smoke from wildland fires, tobacco products, or secondhand smoke are at a higher risk of developing cardiovascular disease.
Air pollution is a significant problem in China, and studies have found a strong association between exposure to ambient air pollutants and respiratory mortality in cities like Xi'an. In 2016, chronic respiratory diseases accounted for 9% of total NCD deaths in China, with approximately 870,000 deaths. Respiratory diseases are expected to become the leading cause of morbidity and mortality by 2030. Globally, air pollution is estimated to cause about 26% of respiratory infection deaths, with people in low- and middle-income countries disproportionately affected.
While the impact of individual risk factors like tobacco smoking, gender, and body mass index on cardiovascular mortality has been studied, adjusting for these factors did not significantly alter the relationship between air pollution and CVD. The American Heart Association (AHA) has published guidelines for healthcare professionals to aid in the primary prevention of cardiovascular disease and stroke, emphasizing multifactorial interventions such as diet, exercise, and smoking cessation.
Natural Air Pollutants: Two Unseen Sources Revealed
You may want to see also

Cancer
Outdoor air pollution is a significant contributor to the global disease burden. Most people live in areas where air pollution levels exceed the World Health Organization's (WHO) health-based air quality guidelines, primarily due to emissions from industry, power generation, transportation, and domestic burning. As a result, outdoor air pollution poses a severe global public health challenge with numerous adverse health effects, including cancer.
Lung cancer is the most commonly diagnosed cancer worldwide and the leading cause of cancer-related deaths. In 2018, there were approximately 2.1 million new cases and 1.8 million deaths, representing 11.6% of all new cancer diagnoses and 18.4% of all cancer deaths globally. The five-year net survival rate for lung cancer is low, ranging from 10% to 20% globally.
Numerous studies have established a positive association between exposure to ambient air pollution and lung cancer incidence and mortality. Fine particulate matter, especially PM2.5, has been identified as a significant contributor to lung cancer risk. A 10 μg/m3 increase in PM2.5 concentrations has been associated with a 9% increase in lung cancer mortality. Additionally, air pollution exposure after a lung cancer diagnosis shortens survival rates. Higher levels of ambient air pollution have been linked to reduced survival in lung cancer patients, particularly those with early-stage tumors and adenocarcinomas.
While lung cancer has been the primary focus of research, recent studies have suggested that air pollution is associated with an increased risk of mortality for several other types of cancer. Positive associations have been found between PM2.5 and NO2 concentrations and colorectal, breast, cervical, bladder, and pancreatic cancer mortality. Additionally, NO2 has been linked to increased mortality from stomach cancer, while O3 has been associated with reduced mortality from colorectal cancer.
Wildfire exposure has also been linked to an increased incidence of lung cancer. A study found that individuals exposed to wildfires within 50 km of their residential locations had a 4.9% higher incidence of lung cancer than the unexposed population.
Air pollution, particularly PM2.5, is now recognized as an established cause of lung cancer, second only to smoking exposure. The International Agency for Research on Cancer classifies outdoor air pollution and PM2.5 as Group 1 carcinogens contributing to lung cancer.
Waste Oil Burning: Clean Air or Pollutant?
You may want to see also

Morbidity
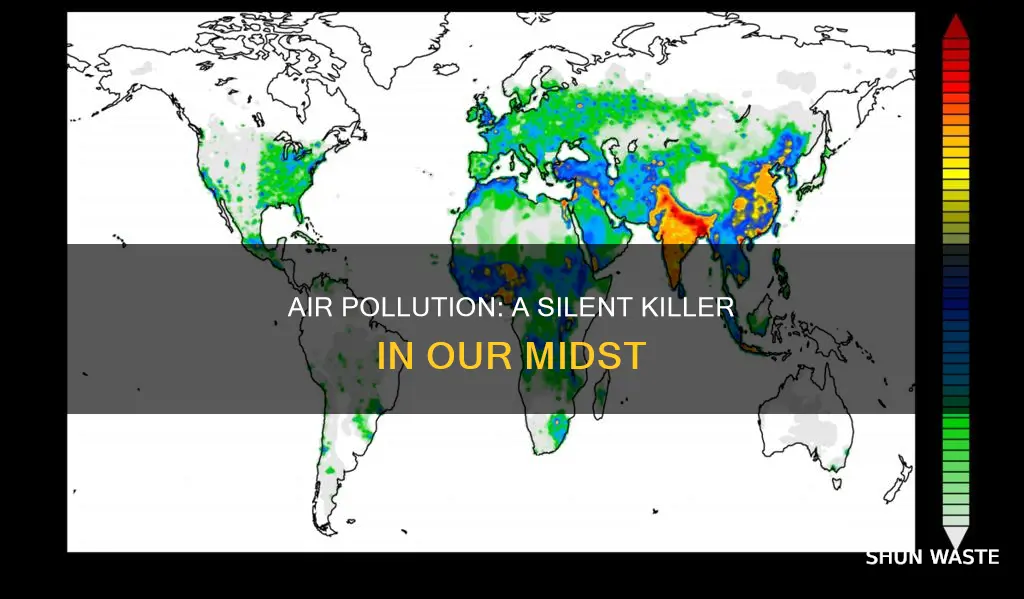
Ambient air pollution is a major cause of morbidity and mortality worldwide. In 2019, it was the largest environmental risk to health, causing an estimated 4.2 million premature deaths globally per year. The World Health Organization (WHO) estimates that 99% of the global population breathes air that exceeds WHO guideline limits on pollutant levels. Low- and middle-income countries suffer the highest exposures, with 89% of premature deaths occurring in these regions.
The health impacts of ambient air pollution are significant and far-reaching. Exposure to fine particulate matter, especially PM2.5 (particulate matter with an aerodynamic diameter of less than 2.5 μm), has been linked to increased morbidity and mortality from multiple health endpoints. Long-term exposure to PM2.5 and other pollutants such as NO2 (nitrogen dioxide) and O3 (ozone) is associated with non-accidental, cardiovascular, non-malignant respiratory, and lung cancer mortality. Even at very low exposure levels, ambient air pollution has significant impacts on public health, contributing to reduced life expectancy and the loss of healthy life years.
Chronic exposure to ambient PM2.5 and ozone has been associated with adverse birth outcomes and increased morbidity and mortality from numerous non-communicable diseases. In 2019, ambient air pollution was responsible for about 20% of deaths from non-communicable diseases, making it the single largest environmental risk factor. More than 50% of these deaths occurred in China and South Asia, with about 20% occurring in high-income countries in Europe and North America.
The impacts of ambient air pollution on morbidity are evident in the high rates of respiratory and cardiovascular diseases observed in affected populations. In 2019, 68% of outdoor air pollution-related premature deaths were due to ischaemic heart disease and stroke, 14% were due to chronic obstructive pulmonary disease, 14% to acute lower respiratory infections, and 4% to lung cancers. These health impacts highlight the urgency of implementing effective policies and interventions to reduce ambient air pollution levels and protect public health.
Addressing ambient air pollution requires coordinated efforts at the local, national, and regional levels. Successful interventions include promoting clean technologies, improving waste management practices, providing access to clean household energy solutions, prioritizing sustainable transport, improving energy efficiency in buildings, and increasing the use of renewable power sources. By implementing these strategies, countries can reduce ambient air pollution, mitigate its health impacts, and promote sustainable development.
Lichen as Air Pollution Sentinels: Nature's Early Warning System
You may want to see also

Environmental risk factors
- Physical factors: These include the layout, design, and amenities of physical workspaces and residential areas. Examples include unmonitored entries, insufficient lighting, and unsecured rooms.
- Chemical factors: These include exposure to pollutants, heavy metals, and chemicals such as pesticides.
- Biological factors: These include exposure to microorganisms, environmental tobacco smoke, and indoor air pollution.
- Work-related factors: These include occupational exposures, such as exposure to hazardous substances or physical hazards in the workplace.
Air pollution is the main environmental risk factor, and it is the fourth-highest risk factor for health overall. It is responsible for about 7 million deaths annually, with almost all (85%) due to non-communicable diseases (NCDs) such as ischemic heart disease, stroke, COPD, asthma, and lung cancer. Ambient air pollution in both cities and rural areas was estimated to cause 4.2 million premature deaths worldwide per year in 2019. WHO data show that almost the entire global population (99%) breathes air that exceeds guideline limits and contains high levels of pollutants, with low- and middle-income countries suffering the highest exposures.
Other environmental risk factors include radiation, noise, land use patterns, work environment, and climate change. Climate change is a significant factor, with heat waves, extreme weather events, and forest fires triggering and exacerbating NCDs. Addressing these environmental risk factors is crucial for protecting public health and reducing the burden of disease.
Air Pollution: India's Most Polluted City
You may want to see also

Socioeconomic status
The impact of air pollution is not evenly distributed, and socioeconomic status plays a significant role in determining the health outcomes of those exposed to it. Research has shown that individuals of low socioeconomic status (SES) are disproportionately affected by air pollution and face higher health risks. This disparity is observed in both developing and developed nations, with low- and middle-income countries bearing the brunt of the health consequences of outdoor air pollution.
Several factors contribute to the higher vulnerability of low-SES communities. Firstly, these communities often reside in areas with higher concentrations of air pollutants. Pollution sources, such as industrial facilities, power plants, and major roadways, tend to be located near disadvantaged communities, increasing their exposure to harmful pollutants. This proximity to pollution sources is further influenced by factors such as racism, class bias, housing market dynamics, and land costs, which disproportionately affect minority and low-income populations.
Secondly, individuals of low SES may experience increased susceptibility to the health effects of air pollution due to various psychosocial stressors. These stressors include financial strain, job insecurity, low control at work, discrimination, and chronic stress. Additionally, low-SES populations tend to have unhealthier lifestyle habits, such as higher smoking rates and lower consumption of fresh fruits and vegetables. They also face barriers to accessing quality healthcare services, which can exacerbate existing health conditions and make them more vulnerable to the adverse effects of air pollution.
The relationship between SES and mortality rates related to air pollution has been observed in studies worldwide. For example, a study of New Jersey residents found a higher risk of premature death from long-term exposure to particle pollution in communities with larger African American populations, lower home values, and lower median incomes. Similarly, studies in Atlanta, Georgia, revealed that particle pollution increased the risk of asthma attacks in zip codes with higher poverty rates and among individuals eligible for Medicaid. These findings highlight the intersectionality of socioeconomic factors and racial or ethnic disparities, with non-white populations facing higher health risks from air pollution.
The triple jeopardy hypothesis provides a framework for understanding the impact of air pollution on low-SES communities. According to this hypothesis, low-SES communities face higher exposure to air pollutants, increased susceptibility to poor health due to psychosocial stressors, and resulting health disparities driven by environmental factors. While the specific mechanisms contributing to these disparities require further study, the existing evidence underscores the urgent need for effective air quality management and policies that address socioeconomic inequalities to mitigate the health risks associated with air pollution.
Hong Kong's Air Pollution: A Critical Concern
You may want to see also
Frequently asked questions
Ambient air pollution is estimated to cause 4.2 million premature deaths worldwide per year. In addition, around 2.4 billion people are exposed to dangerous levels of household air pollution. The combined effects of ambient and household air pollution are associated with 7 million premature deaths annually.
The main causes of death from ambient air pollution are cardiovascular and respiratory diseases, and cancers. WHO estimates that in 2019, 68% of outdoor air pollution-related premature deaths were due to ischaemic heart disease and stroke, 14% were due to chronic obstructive pulmonary disease, 14% were due to acute lower respiratory infections, and 4% were due to lung cancers.
Studies have found that lower educational levels and living in lower socioeconomic contexts increase the risk of mortality associated with air pollution exposure. The main hypotheses are that either poorer individuals are more exposed to air pollution directly in their jobs or living near industrial sources, or that individuals with lower socioeconomic status become more vulnerable to the harmful effects of air pollution due to limited access to healthcare services and healthy food and water.







