Asthma is a chronic inflammatory airway disease with symptoms such as wheezing, dyspnea, coughing, and chest tightness. While air pollution is known to negatively impact asthma outcomes, there is also research suggesting that a person's exposure to toxins could influence their grandchild's epigenetics, thereby increasing the risk of asthma. This is supported by studies showing that grandparental exposure to severe trauma or cigarette smoking is associated with an increased risk of asthma in grandchildren. Furthermore, air pollution can worsen asthma symptoms, leading to increased hospital visits and, in some cases, early death.
| Characteristics | Values |
|---|---|
| Asthma | A chronic respiratory disease characterised by variable airflow obstruction, bronchial hyperresponsiveness, and airway inflammation. |
| Air Pollution | Can trigger asthma symptoms and attacks, especially in children. |
| Risk Factors | Traffic-related air pollution, nitrogen dioxide, and second-hand smoke exposure. |
| Genetic Factors | Epigenetic changes due to stress and exposure to toxins can influence grandchildren's asthma risk. |
| Maternal Factors | Smoking during pregnancy increases the risk of asthma in offspring. |
| Preventative Measures | Educating patients about minimising exposure to air pollution and developing asthma action plans. |
| Research Gaps | Longitudinal intergenerational studies are needed to confirm associations between grandmaternal exposures and asthma risk. |
What You'll Learn
- Air pollutants can irritate the airways, causing swelling and breathing problems
- Exposure to outdoor pollutants can induce asthma symptoms, exacerbations and decreased lung function
- Grandmaternal smoking during pregnancy is linked to an increased risk of asthma in grandchildren
- Maternal trauma may instill asthma susceptibility in children due to epigenetics
- Air pollution is linked to increased hospital visits and can cause early death

Air pollutants can irritate the airways, causing swelling and breathing problems
Asthma is a chronic inflammatory airway disease with symptoms such as wheezing, dyspnea, coughing, and chest tightness. It is characterized by variable airflow obstruction, bronchial hyperresponsiveness, and airway inflammation. While genetics plays a role in the development of asthma, environmental factors can also contribute to it.
Biological contaminants, such as viruses, bacteria, pollen, and animal dander, can also trigger allergic reactions and exacerbate airway diseases like asthma. Additionally, indoor pollutants like tobacco smoke, cooking smoke, and wood-burning stoves contribute to poor air quality, which can trigger asthma symptoms.
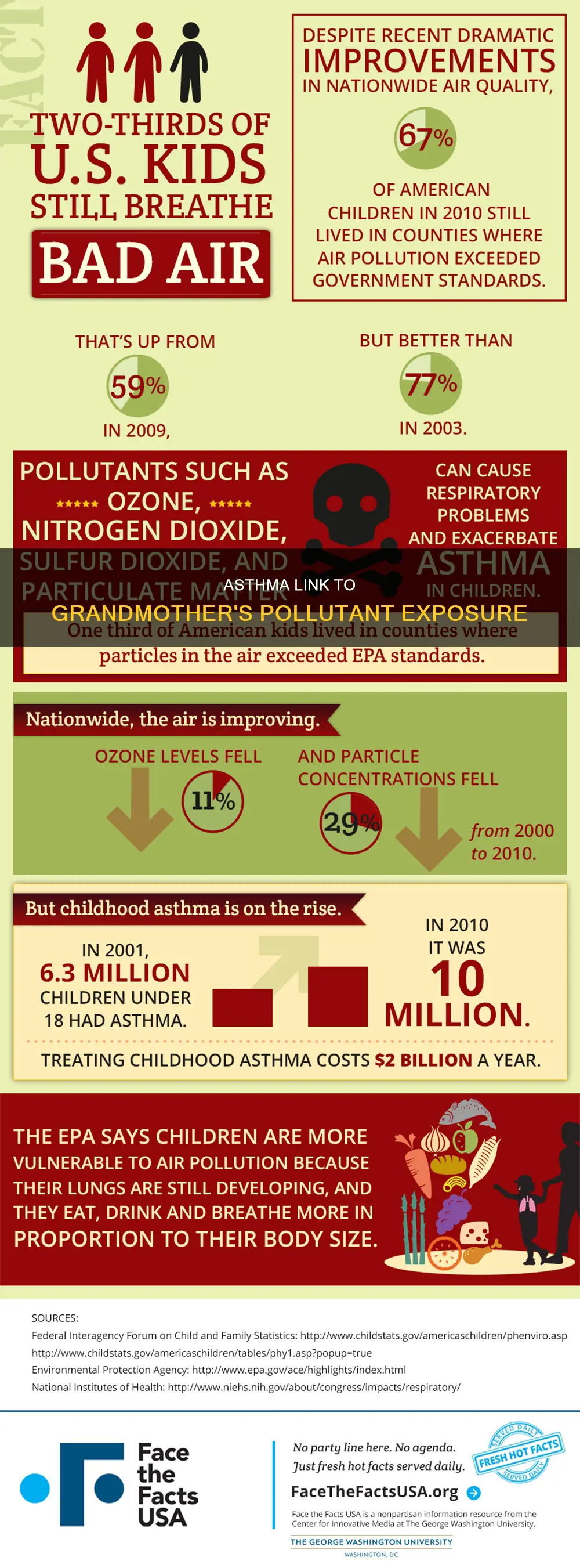
The impact of air pollution on asthma is significant. Exposure to outdoor pollutants can induce asthma symptoms, exacerbations, and decreased lung function. People with asthma are at greater risk from breathing in small particles and irritating gases, and high pollution levels often lead to increased hospital admissions for asthma attacks. Children are especially vulnerable, as their lungs are still developing, and they breathe faster, taking in more polluted air. Older individuals with long-term lung conditions are also at higher risk.
While the causal relationship between air pollution and adult asthma development requires further research, there is evidence that air pollution negatively affects asthma outcomes in both adult and pediatric populations. Understanding the impact of air pollution on asthma is crucial for physicians to educate patients about minimizing exposure and managing their asthma effectively. Additionally, raising awareness about the effects of air pollution can prompt public health authorities and governments to implement measures to reduce exposure to harmful pollutants.
The Pink Sky Conundrum: Pollution or Natural Wonder?
You may want to see also

Exposure to outdoor pollutants can induce asthma symptoms, exacerbations and decreased lung function
Asthma is a chronic inflammatory airway disease with symptoms such as wheezing, dyspnoea, coughing, and chest tightness. It is characterized by variable airflow obstruction, bronchial hyperresponsiveness, and airway inflammation. While genetics plays a role in the development of asthma, exposure to outdoor pollutants can also induce asthma symptoms, exacerbations, and decreased lung function.
Outdoor air pollution, such as ozone, nitrogen dioxide, and carbon monoxide, can irritate the airways and lungs, triggering asthma attacks and worsening symptoms in those who already have asthma. People with asthma are particularly vulnerable to the effects of air pollution, and poor air quality can be a significant trigger for asthma flare-ups. Exposure to outdoor pollutants can also increase the risk of developing asthma, with evidence suggesting that air pollution has a negative impact on asthma outcomes in both adult and pediatric populations.
Research has found that short-term and long-term exposure to high levels of carbon monoxide, nitrogen dioxide, and PM 2.5 is associated with alterations in genes that regulate the immune system's ability to differentiate allergens from dangerous foreign substances. These genetic alterations are significantly associated with asthma, providing insight into the epigenetic effects of air pollutant exposure.
Additionally, studies have suggested that experiences in the womb or even before conception can impact the offspring's susceptibility to asthma. For example, maternal smoking during pregnancy is associated with an increased risk of asthma in the child. This intergenerational impact may be due to epigenetic changes, where environmental factors like stress, toxins, and nutrition can alter DNA, protein production, and cell behavior.
Furthermore, stress has been identified as a potential factor in the development of asthma. Chronic stress can trigger illness, and exposure to stressful events or trauma during pregnancy may increase the risk of asthma in grandchildren. While the exact mechanisms are not yet fully understood, the field of epigenetics offers a potential explanation for these intergenerational associations.
Understanding Particulate: What Does It Mean?
You may want to see also

Grandmaternal smoking during pregnancy is linked to an increased risk of asthma in grandchildren
Asthma is a chronic inflammatory airway disease with symptoms such as wheezing, dyspnoea, coughing, and chest tightness. It is characterized by variable airflow obstruction, bronchial hyperresponsiveness, and airway inflammation. While air pollution has been linked to adverse asthma outcomes in both adults and children, recent research has also implicated grandmaternal smoking during pregnancy as a risk factor for asthma in grandchildren.
The impact of smoking during pregnancy on the development of asthma in the first generation of offspring (F1) has been well-established. However, the intergenerational effects on the F2 generation have been less extensively studied. Recent studies have begun to explore the potential link between grandmaternal smoking during pregnancy and the risk of asthma in grandchildren.
One of the earliest human studies found a higher risk of early childhood asthma when maternal grandmothers smoked during pregnancy, independent of maternal smoking. This study suggested that grandmaternal smoking during the mother's fetal period could increase the likelihood of asthma in her grandchildren. Subsequent research has further explored this association, with conflicting results. While some studies have supported the initial findings, others have found no significant associations.
A study conducted in Southern California investigated the associations of maternal and grandmaternal smoking before, during, and after pregnancy with childhood asthma. The results indicated that in utero exposure to maternal smoking was associated with an increased risk of asthma diagnosed in the first five years of life. Similarly, grandmaternal smoking during pregnancy was linked to a higher risk of asthma in grandchildren, specifically in male grandchildren. This study highlighted the deep-rooted and long-lasting effects of tobacco smoking across generations.
The Lifelines cohort study, a prospective longitudinal three-generation cohort study in the Netherlands, also examined the association between grandmaternal smoking during pregnancy and asthma risk in grandchildren. This study found that grandmaternal smoking during pregnancy was associated with lower lung function in grandchildren, particularly in male grandchildren, which paralleled the higher risk of asthma in this group. However, another study investigating paternal grandmaternal smoking during pregnancy found no significant association with asthma in grandchildren.
While the research on grandmaternal smoking during pregnancy and asthma risk in grandchildren is limited and somewhat conflicting, it highlights the potential intergenerational impact of environmental factors on health outcomes. Further studies are needed to better understand the complex interplay between genetics and the environment in the development of asthma and other diseases.
Electric Scooters: Green or Polluting Menace?
You may want to see also

Maternal trauma may instill asthma susceptibility in children due to epigenetics
Asthma is a common respiratory disease that affects people of all ages, with an estimated global prevalence of 1-18%. It is characterised by symptoms such as wheezing, dyspnoea, coughing, and chest tightness, along with variable airflow obstruction, bronchial hyperresponsiveness, and airway inflammation. While the exact mechanisms of asthma are not fully understood, both genetic and environmental factors play a significant role in its development and pathogenesis.
Maternal trauma and chronic stress have been suggested as potential factors that can increase asthma susceptibility in children. This idea is explored in the context of epigenetics, which refers to the study of how environmental factors like stress, toxins, and nutrition can alter DNA expression and cell behaviour without changing the DNA sequence. Research indicates that epigenetic changes can cross generations, meaning a mother's environment and experiences could potentially influence her child's asthma risk. For example, studies have shown that exposure to tobacco smoke during pregnancy or early childhood increases asthma risk, and chronic stress may have a similar effect.
While the link between maternal trauma and asthma susceptibility is not yet fully understood, there is evidence to suggest that epigenetic alterations may occur in the embryo of pregnant asthmatic women, potentially leading to severe asthma in their offspring. Maternal obesity has also been implicated as a factor influencing offspring health, mediated in part through epigenetic changes such as DNA methylation. These findings highlight the complex interplay between environmental exposures, genetics, and epigenetics in the development of asthma.
Additionally, it is important to consider the impact of air pollution on asthma outcomes. Pollutants, particularly traffic-related air pollution, have been shown to negatively affect both adult and paediatric asthma populations. Poor air quality can trigger asthma flare-ups, irritate airways, and increase susceptibility to upper respiratory infections. As a result, physicians are encouraged to ask patients about their exposure to pollutants to help manage their asthma effectively.
In conclusion, while the role of maternal trauma in asthma susceptibility due to epigenetics requires further study, it is a promising field that may provide insights into the complex nature of asthma development. Understanding the interplay between genetics, epigenetics, and environmental factors will hopefully lead to improved diagnostic tools, treatments, and interventions for asthma in the future.
The Beauty of Sunsets: Pollution's Silver Lining
You may want to see also

Air pollution is linked to increased hospital visits and can cause early death
Asthma is a chronic inflammatory airway disease. It is characterized by respiratory symptoms such as wheezing, dyspnea, coughing, and chest tightness. These symptoms are associated with variable expiratory airflow limitation. The prevalence of asthma is estimated to be between 1% and 18% of the population across different countries.
Research has shown that air pollution has a negative impact on asthma outcomes in both adult and pediatric populations. Exposure to outdoor pollutants can induce asthma symptoms, exacerbations, and decreases in lung function. Traffic-related air pollution, nitrogen dioxide, and second-hand smoke exposures represent significant risk factors for asthma development in children.
Air pollution is a major cause of concern for people with asthma. Poor air quality can trigger flare-ups, irritate the airways, and cause breathing problems. Pollutants in the air can make children more susceptible to upper respiratory infections, which can, in turn, bring on asthma symptoms. If allergens in the air are an asthma trigger, pollutants can further increase the sensitivity of the lungs to them.
While the causal relation between air pollution and the development of adult asthma is not yet clearly established, air pollution is detrimental to respiratory health and can worsen asthma symptoms. People with pre-existing respiratory illnesses such as asthma are more vulnerable to the effects of air pollution.
Emerging research in the field of epigenetics suggests that environmental factors like stress, exposure to toxins, and nutrition can alter DNA, protein production, and cell behavior. This means that a person's lifestyle and exposure to toxins could influence their grandchild's epigenetics. Maternal trauma may instill asthma susceptibility in a child due to epigenetics. While most of this research has been conducted on rodents, it could have implications for humans in the future.
Leaf Blowers: Legal, but Are They Noise Polluters?
You may want to see also
Frequently asked questions
Asthma is a chronic inflammatory airway disease characterized by respiratory symptoms such as wheezing, dyspnea, coughing, and chest tightness associated with variable expiratory airflow limitation.
Air pollution can cause asthma and other lung diseases. It can also worsen asthma symptoms, leading to increased hospital visits. Pollutants in the air irritate the airways, causing swelling and tightness, and triggering breathing problems.
Pollutants that can affect people with asthma include ground-level ozone, nitrogen dioxide, sulfur dioxide, carbon monoxide, and particulate matter (PM), especially the smallest particles (PM2.5).
People with asthma can protect themselves from air pollution by checking daily air quality reports and limiting time outdoors when levels are unhealthy. They can also reduce allergens and irritants in their homes, such as smoke, scented products, and mold.
There may be a link between a grandmother's exposure to pollutants and asthma in her grandchildren. Research suggests that epigenetic changes can cross generations, meaning a person's environment might influence their grandchild's epigenetics. While most studies have been conducted on rodents, some findings indicate that grandmaternal smoking during pregnancy is associated with an increased risk of asthma in grandchildren.







